8th Postgraduate Course for Training in Reproductive Medicine and Reproductive Biology
Single-dose Antibacterial Treatment for Asymptomatic Bacteriuria in Pregnancy
C. Diculescu
Romania
Tutors
O. Irion and M. Boulvain
Department of Obstetrics and Gynecology
Geneva University Hospital
Abstract
Asymptomatic bacteriuria occurs in about one in 20 pregnant women and it is an important risk factor for developing acute symptomatic infection later in pregnancy, which occurs in about one in four women with asymptomatic bacteriuria. Treatment of bacteriuria prevents up to 80 percent of cases from pyelonephritis. Numerous studies have shown that single-dose antibiotic treatment for asymptomatic bacteriuria is as effective as long course treatments. Published results of single dose treatment for urinary tract infection in pregnant women differ widely with regard to diagnostic methods and duration of follow -up. Single-dose treatment, being as effective as conventional treatment, has the advantages of minimal medication, of increased patient compliance, reduced cost, reduction of side-effects and increased safety. The treatment should be based on antibiotic susceptibility testing. Urine cultures should be repeated seven days following therapy to assess cure or failure. Failure to eliminate bacteriuria with repeated therapy (short- or long-term regimen) or recurrence with the same organism is indicative of renal parenchymal infection or a structural abnormality. These women should have follow-up urine cultures and urology evaluation after delivery.
Asymptomatic bacteriuria, defined as persistent bacterial colonization of the urinary tract in the absence of specific symptoms, occurs in 4 to 7 percent of pregnancies, 11,14 about one in 20 pregnant women. It is an important risk factor for developing acute symptomatic infection later in pregnancy, which occurs in about one in four women with bacteriuria17.
Undiagnosed and untreated bacteriuria in pregnancy represents a considerable risk factor for acute pyelonephritis in approximately 5% of pregnant women. It may increase the risk of low-birth-weight babies and is also associated with an increased risk of perinatal fetal death 10,19. Treatment of bacteriuria prevents up to 80 percent of cases of pyelonephritis 11.
The prevalence of infection is strongly related to socioeconomic status and is similar in both pregnant and non-pregnant women 14,18. In non-pregnant women, asymptomatic bacteriuria may not have a significant impact and may not be persistent. During pregnancy, however, bacteriuria is more likely to be persistent due to dilated ureters, influence of hormonal changes and increase in bladder capacity. A decrease in the concentrating ability of the kidney may also cause a decrease in the natural antibacterial activity of urine. Glucosuria during pregnancy also contribute to the risk to develop bacteriuria14. Bacterial growth is also favored by the increased urinary content of aminoacids, vitamins and other nutrients 13.
It has been shown that for most women with bacteriuria at delivery it has been present at the first antenatal visit. In approximately 1% to 2% of women bacteriuria is acquired later in pregnancy. The risk to acquire bacteriuria during pregnancy increases with gestational age from 0.8% in the twelfth week to 1.93% at the end of pregnancy 14 . In a large trial conducted in 3254 pregnant women the optimal time for screening for bacteriuria was found to be at sixteen weeks of gestation14.
Concerning the etiology of bacteriuria, most organisms recovered by routine culture techniques continue to be coliform bacteries with E.Coli the most common by far14,18. Also, bacteriuria in pregnancy usually reflects prior colonization, e.g. at the time of onset of sexual activity, rather than acquisition during pregnancy itself 14.
Objectives
To establish whether single-dose antibacterial treatment for asymptomatic bacteriuria in pregnancy is efficient compared to short-term (3-10 days), long-term (14-21 days) and continuous treatment (treatment continued until delivery).
Data sources
An English-language literature search, employing Medline, The Cochrane Library and bibliographic review of the references obtained, was performed (key terms : urinary tract infections, bacteriuria , pregnancy, single-dose therapy, short-term therapy)
Study selection and data extraction
Studies, dealing with the treatment of bacteriuria in pregnancy were identified. Comparison of the results of single-dose treatment of urinary tract infections in pregnant women is difficult due to the different methods of diagnosis and duration of follow -up.
Main results
Extensive studies regarding the natural history of bacteriuria in pregnancy have provided the rational for the treatment of asymptomatic bacteriuria in pregnancy. The development of symptomatic infection in an individual patient, however, cannot be predicted, although persistent bacteriuria despite treatment is associated with the development of a symptomatic infection 14.
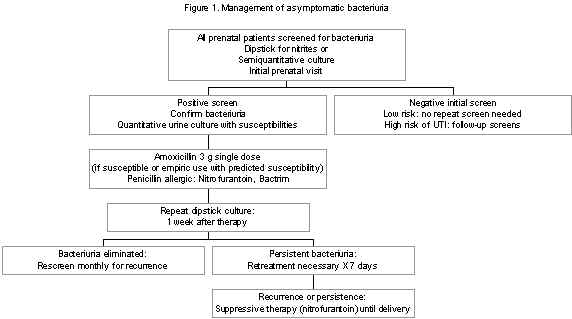
The authors’ approach to the management of asymptomatic bacteriuria in pregnancy is shown in Figure 1 14.
An initial screening culture should be performed on all pregnant women at the first prenatal visit, preferably in the first trimester. A dipstick culture is an inexpensive and an accurate method for initial screening. Women with a negative screening culture can be followed up by routine antenatal care; however, women with a history of recurrent urinary tract infections may be at higher risk for developing infection later in pregnancy, despite an initial negative culture. The authors routinely repeat the culture at the beginning of the third trimester. A positive dipstick should be confirmed with a quantitative culture, which also allows for identification of the organism and antimicrobial susceptibility testing. A serum creatinine measurement is also recommended for those patients with positive urine cultures 14.
The duration of therapy for bacteriuria in pregnancy has received much attention.
Early studies used continuous therapy until term 14. After that, shorter courses of therapy have been shown to be as effective as continuous therapy. Although therapy should be guided by antibiogram, many short-course regimens have been shown to be effective in eliminating bacteriuria of pregnancy (Table 1) 1,4,5,614,15,16,19,20,21.
Approximately 70% to 80% of the patients initially treated with 7 to 10 days of therapy have eliminated bacteriuria. A similar efficacy rate has been reported following 3-day regimens.
Other studies have evaluated single-dose therapy for bacteriuria in pregnant women (Table 1). Although most of the organisms isolated are susceptible to ampicillin, which is well tolerated in many patients, the treatment should be based on antibiotic susceptibility testing .
Also, ampicillin has been extensively used in pregnancy and does not seem to be harmful to mother or fetus 1,14. Amoxicillin is effective and well tolerated ; the authors prefer a 3 or 7-day course of 250 mg three times daily as initial therapy, although a single dose of 3 g has been reported as effective 3,8,14,15,20.
Nitrofurantoin is an equally effective and non-toxic regimen in patients who are allergic to penicillin or in patients infected with resistant organisms. Nitrofurantoin has been given as a single 200 mg dose or 100 mg four times a day for 3 or 7 days 3,14,20,21.
Sulfisoxazole at 1g followed by 0.5 g every 6 hours for 7 days is a traditional regimen and may also be effective in a single dose of 2 g. Sulfisoxazole should probably not be used near term because of possible hyperbilirubinemia in the neonate. Nitrofurantoin and sulfisoxazole are occasionally associated with hemolytic anemia caused by glucose-6-phosphate dehydrogenase deficiency 14.
Single-dose or short-course therapy with other agents, including cephalexin, amoxicillin-clavulanic acid, trimethoprim-sulfamethoxazole and fosfomycin are also effective 3,4,11,14,15,16,17,20. Ofloxacin appears to be more effective for short term therapy compared to trimethoprim-sulfamethoxazole treatment. 4.
If the organism is susceptible to cephalexin or nitrofurantoin, postcoital prophylaxis with either agent for the remainder of pregnancy may be beneficial19 .
Treatment failures with single-dose or short-course therapy result from resistance of the infecting organisms or the presence of renal infection.
Localization of asymptomatic bacteriuria (bladder or renal bacteriuria), despite the studies which have been shown to correlate with the pattern of recurrence after treatment, does not contribute to the management of pregnant women, since overall recurrence rates are independent of the site of infection 12.
A follow-up urine culture should be done approximately one week after therapy. If the urine is sterile, the woman should be followed up with monthly urine cultures until delivery. If single-dose or short-course therapy fail to clear the infection, a repeat 7 to 10-day course of therapy with a different agent chosen on susceptibility should be given. Patients who don’t respond to two courses of therapy are recommended a suppressive therapy with an agent to which the organism is susceptible, such as nitrofurantoin, 50 to 100 mg at night until delivery. Follow-up cultures should be done in all women with recurrent or persistent bacteriuria after delivery and examination of the urinary tract should be undertaken 3 to 6 months after delivery 14.
Discussion
The important issue is not the length of therapy chosen but that appropriate follow-up is obtained to document the elimination of bacteriuria.
Any method to predict which patient will respond to a single-dose treatment would be inaccurate. Absence of symptoms is not predictive of therapeutic result. At present, there is no method to identify those patients who don’t respond to the treatment13,14.
The only way of detecting failure of treatment is careful microbiological follow-up.
The single-dose regimen has the advantages of increased patient compliance and reduced costs, reduction in side-effects and increased safety.
Single-dose therapy of bacteriuria in pregnancy has advantages in addition to that of minimal medication. The low incidence of induced bacterial resistance reduces the problem of perinatal infection with resistant organisms. Monilial vaginitis may be found in 25% of women treated with a broadspectrum antibiotic, but is unlikely to appear with single-dose treatment. Other side-effects are less common, therefore the compliance for treatment and follow-up is good.
The physiological increase in glomerular filtration rate, which may be as much as 50%, increases the speed of renal excretion of drugs. Therefore, drugs best suited for single-dose treatment of urinary tract infection are preparations excreted via the urine over a longer time. Also the very common polyuria reduces the time a drug spends in the urinary tract 13.
Appropriate antimicrobial drugs include penicillins, cephalosporins and nitrofurantoin 16.
There are, however, advantages in studying treatment during pregnancy. The mothers are usually healthy. Bacteria infecting them tend to reflect community organisms rather than resistant hospital flora. Long-term follow-up is possible because the mothers are motivated and they are seen regularly and frequently from early in pregnancy until 6 weeks after delivery 13,14.
Conclusions
Asymptomatic bacteriuria in pregnancy can be treated with a single dose of an antimicrobial agent to which the organism is susceptible.
Urine cultures should be repeated seven days following therapy to assess cure or failure.
Failure to eliminate bacteriuria with repeated therapy (short- or long-term regimen) or recurrence with the same organism is indicative of renal parenchymal infection or a structural abnormality. All these women should have follow-up cultures and an urology evaluation after delivery.
References
- Adelson MD, Graves WL, Osborne NG: Treatment of urinary infections in pregnancy using single versus 10-day dosing. J Natl Med Assoc 84(1) :73-75,Jan 1992
- Bailey RR, Bishop V, Peddie BA: Comparison of single dose a 5-day course of co-trimoxazole for asymptomatic (covert) bacteriuria of pregnancy. Aust N Z J Obstet Gynaecol 23(3) :139-141, Aug 1983
- Bint AJ, Hill D : Bacteriuria of pregnancy - an update on significance, diagnosis and management. J Antimicrob Chemother 33 Suppl A :93-97, May 1994
- Block JM, Walstad RA, Bjertnaes A, Hafstad PE, Holte M, Ottemo I, Svarva PL, Rolstad T, Peterson LE: Ofloxacin versus trimethoprim-sulphamethoxazole in acute cystitis. Drugs 34 Suppl 1:100-106, 1987
- Brumfitt W, Franklin I, Hamilton-Miller J, Anderson F: Comparison of pivmecillinam and cephradine in bacteriuria in pregnancy and in acute urinary tract infection. Scand J Infect Dis 11(4) :275-279, 1979
- Faro S, Pastorek JG 2d, Plauche WC, Korndorffer FA, Aldridge KE: Short-course parenteral antibiotic therapy for pyelonephritis in pregnancy. South Med J 77(4) :455-457, Apr 1984
- Garland SM, O’Reilly MA : The risks and benefits of antimicrobial therapy in pregnancy. Drug Saf 13(3) :188-205, Sep 1995
- Gerstner GJ, Muller G, Nahler G : Amoxicillin in the treatment of asymptomatic bacteriuria in pregnancy : a single dose of 3 g amoxicillin versus a 4-day course of 3 doses 750 mg amoxicillin. Gynecol Obstet Invest 2716 :84-87, 1989
- Grio R, Porpiglia M, Vetro E, Uligini R, Piacentino R, Mini D, Marchino GL : Asymptomatic bacteriuria in pregnancy : a diagnostic and therapeutic approach. Panminerva Med 36(4) :195-197, Dec 1994
- Grio R, Porpiglia M, Vetro E, Uligini R, Piacentino R, Mini D, Marchino GL: Asymptomatic bacteriuria in pregnancy :maternal and fetal complications. Panminerva Med 36(4):198-200,Dec 1994
- Kiningham RB : Asymptomatic bacteriuria in pregnancy. Am Fam Physician 47(5) :1232-1238
- Leveno KJ, Harris RE, Gilstrap LC, Whalley PJ, Cunningham FG: Bladder versus renal bacteriuria during pregnancy: recurrence after treatment. Am J Obstet Gynecol Feb 15 ;139(4) :403-406, 1981
- McFadyen IR, Campbell-Brown M, Stephenson M, Seal DV: Single-dose treatment of bacteriuria in pregnancy. Eur Urol 13 Suppl 1 :22-25, 1987
- Patterson TF, Andriole VT: Detection, significance, and therapy of bacteriuria in pregnancy. Update in the managed health care era. Infect Dis North Am 11(3):593-608, Sep 1997
- Pedler SJ, Bint AJ: Comparative study of amoxicillin-clavulanic acid and cephalexin in the treatment of bacteriuria during pregnancy. Antimicrob Agents Chemother 27(4):508-510, Apr 1985
- Pedler SJ, Bint AJ : Management of bacteriuria in pregnancy.Drugs 33(4) :413-421, Apr 1987
- Reeves DS: Treatment of bacteriuria in pregnancy with single dose fosfomycin trometamol : a review. Infection 20 Suppl 4 :S313-S316, 1992
- Smaill F: Antibiotic vs no treatment for asymptomatic bacteriuria in pregnancy (Cochrane Review) In : The Cochrane Library, Issue 3, 1998. Oxford : Update Software
- Tan JS, File TM Jr: Treatment of bacteriuria in pregnancy. Drugs 44(6) :972-980, Dec 1992
- Vercaigne LM, Zhanel GG : Recommended treatment for urinary tract infection in pregnancy. Ann Pharmacother 28 (2) :248-251,Feb 1994
- Whalley PJ, Cunningham FG: Short-term versus continuous antimicrobial therapy for asymptomatic bacteriuria in pregnancy. Obstet Gynecol 49(3) :262-265, Mar 1977
- Zinner SH: Management of urinary tract infections in pregnancy :a review with comments on single dose therapy.Infection 20 Suppl 4: S280-S285,1992
Table 1. Effective regimens for asymptomatic bacteriuria in pregnancy
| AMOXICILLIN | 250 mg tid x 7 days 250 mg tid x 3 days 3 g single dose 3 g followed by 3 g 12 h later 2 g single dose plus 1 g probenecid |
Well tolerated, extensive clinical use in pregnancy. Empiric use with predicted susceptibility; high urinary concentrations |
| AMPICILLIN | 3.5 g single dose plus 1 g probenecid | Not so effective |
| NITROFURANTOIN | 100 mg qid x 7 days 100 mg qid x 3 days 200 mg single dose |
Risk of hemolytic anemia with G6PD deficiency |
| SULFISOXAZOLE | 1 g followed by o.5 g qid x 7 days 2 g single dose |
Associated with hyperbilirubinemia near term |
| CEPHALEXIN | 1 g d x 3 days 2 g single dose 2 g single dose plus 1 g probenecid |
Some studies report slightly lower cure rates |
| AMOXICILLIN / CLAVULANIC ACID | 250 mg/125 mg tid x 7 days | Little experience in pregnancy, expensive |
| TRIMETHOPRIM (TMP) / SULFAMETHOXAZOLE (SXT) | TMP 32o mg/SXT 1600 mg x 1 dose or 3 days | Use with caution in pregnancy because of question of teratogenity; avoid use in third trimester |
| FOSFOMYCIN TROMETAMOL | 3 g single dose | Little experience in pregnancy |
| OFLOXACIN | 100 mg tid x 3 days | Well tolerated |